Differences Between Diabetic Retinopathy and Macular Edema
Diabetes and Eye Health: Understanding Diabetic Retinopathy and Diabetic Macular Edema
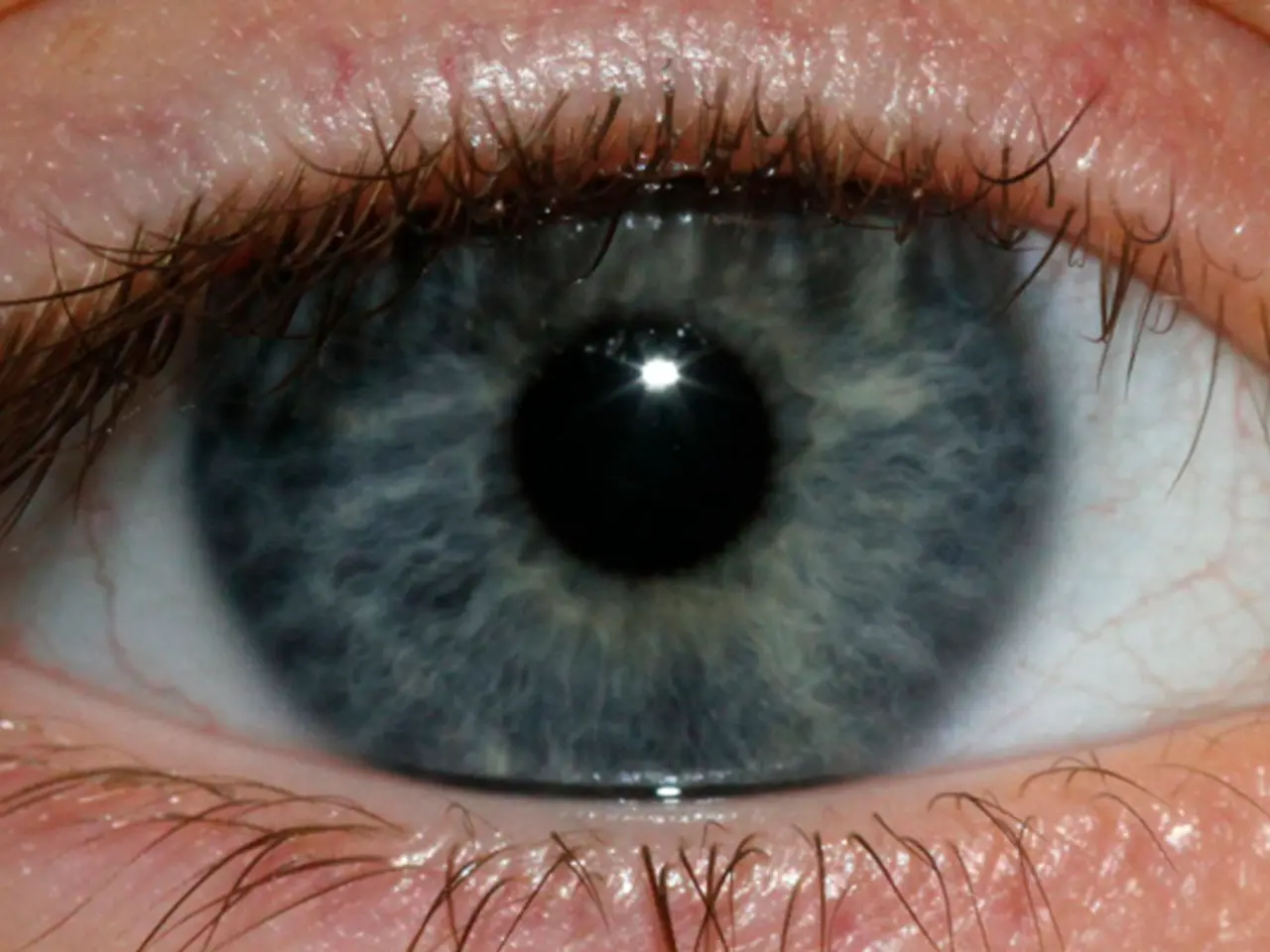
Diabetes can lead to serious eye problems, including Diabetic Retinopathy (DR) and Diabetic Macular Edema (DME). These conditions affect the health and function of the retina, the thin layer of tissue at the back of the eye, and can cause vision loss if left untreated.
Diabetic Retinopathy (DR) is a diabetes-related retinal disease characterized by damage and weakening of blood vessels in the retina. This condition can cause the vessels to leak, break down, or grow abnormally, potentially leading to vision problems such as blurry or wavy vision, difficulty seeing in low light, floaters, or loss of peripheral vision.
Diabetic Macular Edema (DME), on the other hand, is a specific complication of DR. It refers to the swelling of the macula—the central part of the retina responsible for sharp, central vision—due to fluid leaking from damaged retinal blood vessels. This fluid buildup causes the macula to swell, leading to distorted vision, colors appearing washed out, or central vision loss.
Relationship and Development
DME develops as a consequence of diabetic retinopathy when damaged blood vessels leak fluid into the macula. Not all diabetic retinopathy patients develop DME, but DME is one of the most serious vision-threatening complications of diabetic retinopathy. Both conditions are caused by high blood sugar levels causing inflammation and damage to retinal blood vessels, leading to leakage and swelling.
Differences
While diabetic retinopathy affects the retina broadly, DME specifically affects the macula area. The primary issue in DR is blood vessel damage, leakage, and/or abnormal growth, whereas in DME, the issue is macular swelling due to fluid accumulation. Vision impact also differs, with DR causing peripheral vision loss, blurry vision, floaters, and DME causing central vision distortion, blurred or washed-out colors, or central vision loss.
Prevention and Management
Prevention of both conditions lies in managing blood sugar, blood pressure, and cholesterol levels tightly. Annual eye exams are essential for early detection of both conditions to prevent progression. Treatment of diabetic retinopathy aims to prevent or slow blood vessel damage, while treatment of DME includes intravitreal injections of anti-VEGF agents to reduce vessel leakage and swelling, laser therapy to seal leaking vessels, or surgery in severe cases.
In summary, diabetic retinopathy damages retinal blood vessels broadly, while diabetic macular edema is the swelling of the macula caused by this damage. DME is a direct complication arising from retinopathy, and their prevention and management overlap, focusing on good diabetes control and eye monitoring.
Yearly eye exams are essential for a person living with diabetes to check their eye health and identify any conditions in the early stages. If a person living with diabetes begins to notice changes to their vision, such as blurriness, they should attend an eye exam immediately. By managing their diabetes effectively and attending regular eye exams, individuals can significantly reduce their risk of vision loss due to DR or DME.
Science plays a crucial role in understanding and addressing diabetes-related medical conditions, such as Diabetic Retinopathy (DR) and Diabetic Macular Edema (DME). These chronic diseases are unrelated to workplace-wellness initiatives, but addressing them contributes to overall health-and-wellness.
Given that DR is a diabetes-related retinal disease that causes blood vessels in the retina to leak, break down, or grow abnormally, it can lead to various vision problems like blurry vision, difficulty seeing in low light, floaters, and loss of peripheral vision. DME, on the other hand, is a specific complication of DR that affects the macula, causing it to swell due to fluid leaking from damaged retinal blood vessels. This leads to distorted vision, colors appearing washed out, or central vision loss.
Manufacturing, mental-health, skin-care, and energy industries, among others, have their unique demands and challenges; however, managing chronic-diseases like diabetes and its related complications such as DR and DME should be an integral part of every individual's lifestyle, regardless of their industry.
DME develops as a consequence of diabetic retinopathy when damaged blood vessels leak fluid into the macula. Both conditions share common causes—high blood sugar levels inflaming and damaging retinal blood vessels, leading to vessel leakage and swelling. While DR affects the retina broadly, DME specifically impacts the macula area.
In terms of differences, the primary issue in DR is blood vessel damage, leakage, and/or abnormal growth, whereas in DME, the issue is macular swelling due to fluid accumulation. The impact on vision also differs, with DR causing peripheral vision loss, blurry vision, floaters, and DME leading to central vision distortion, blurred or washed-out colors, or central vision loss.
Preventing both conditions relies on managing blood sugar, blood pressure, and cholesterol levels effectively. Regular eye exams are essential for early detection of both conditions to prevent their progression. Treatments for diabetic retinopathy aim to prevent or slow blood vessel damage, while treatments for DME include intravitreal injections and laser therapy.
It is vital for entrepreneurs, retailers, and small-business owners to understand the importance of health-and-wellness in their industries and promote workplace-wellness, focusing on chronic-disease management, such as diabetes, respiratory-conditions, digestive-health, and eye-health.
People with diabetes must invest in their health and wellbeing by maintaining fitness-and-exercise routines, following nutrition guidelines, and ensuring cardiovascular-health. Balanced diets and regular exercise can help manage diabetes and reduce the risk of diabetes-related complications.
Financial management is also crucial as individuals may need to allocate funds for therapies-and-treatments in case of diabetes-related complications. Factors like finance, retirement planning, and wealth-management are essential in ensuring one's durable lifestyle in the long run.
Individuals living with diabetes must also prioritize mental-health, even as they focus on physical health. Stress management techniques, therapy, and medication can help manage mental-health issues.
Information and education on diabetes and its complications can help manage diabetes better, ensuring timely identification and appropriate treatment. Insurance coverage and services play a crucial role in managing diabetes and its complications, making banking-and-insurance a vital aspect of diabetes management.
Technology plays a significant role in diabetes management, with wearables and smart home-devices providing real-time monitoring of blood glucose levels. Data-and-cloud-computing also enables sharing data with healthcare providers, ensuring timely intervention and management.
Health-conscious lifestyles involve not only managing diabetes and other chronic-diseases but also focusing on eye-health, skin-care, and general well-being. Gardening, budgeting, and technology can contribute to overall well-being, promoting a healthy lifestyle that is essential for individuals with diabetes and chronic-kidney-disease, cancer patients, or those with respiratory-conditions, neurological-disorders, autoimmune-disorders, or skin-conditions.
In summary, individuals living with diabetes must prioritize their health, including managing their diabetes, maintaining physical fitness-and-exercise routines, following nutrition guidelines, and scheduling regular eye exams to prevent vision loss due to DR or DME. Early detection and timely intervention can significantly reduce the risk of vision loss, emphasizing the importance of ongoing health monitoring.
Individuals managing diabetes should also prioritize mental-health, stress management techniques, and financial management to ensure a balanced and durable lifestyle. Emphasis should also be placed on lifestyle choices, including smart choices in housing-market, investing, personal-finance, and career paths that promote overall well-being and reduce the risk of diabetes complications.
Lastly, entrepreneurs, small-business owners, and industry leaders should promote workplace-wellness, focusing on health-and-wellness initiatives that cater to managing chronic diseases, supporting access to affordable healthcare, and promoting a culture of diversity-and-inclusion that embraces health-conscious lifestyle choices. By prioritizing these aspects, industry leaders can contribute to better workplace wellness, create safer and healthier work environments that encourage employees to thrive both personally and professionally.